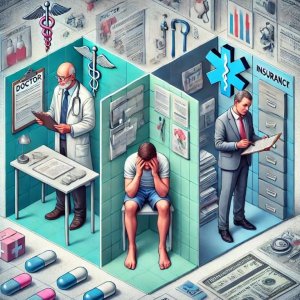
 Modern medicine has achieved extraordinary advancements in diagnosis and treatment. Yet, many patients and doctors alike find themselves frustrated with how fragmented the system has become. Nowhere is this frustration more evident than in the realm of insurance and the compartmentalized approach to patient care. The result? Healthcare that often feels like a trip to the parts department at an auto shop, rather than a cohesive journey toward health.
Modern medicine has achieved extraordinary advancements in diagnosis and treatment. Yet, many patients and doctors alike find themselves frustrated with how fragmented the system has become. Nowhere is this frustration more evident than in the realm of insurance and the compartmentalized approach to patient care. The result? Healthcare that often feels like a trip to the parts department at an auto shop, rather than a cohesive journey toward health.
The Insurance Headache: A Shared Burden
For both patients and providers, navigating insurance is a constant struggle. Patients face opaque policies, endless paperwork, and surprising out-of-pocket costs, often for essential treatments. Meanwhile, doctors find their hands tied by pre-authorizations, billing codes, and restrictions that limit their ability to deliver personalized care.
Insurance companies have become gatekeepers, dictating what care patients can receive based on a narrow framework of what is deemed “medically necessary.” This bureaucracy not only undermines trust but also shifts the focus away from the patient’s actual needs. Doctors, drained by administrative tasks, have less time to connect with their patients, exacerbating the sense of dissatisfaction on both sides.
The “Parts Department” Mentality in Medicine
Imagine your body as a car. You’re experiencing an issue with the engine, so you visit a specialist who only handles spark plugs. Another doctor might only deal with the transmission. While each specialist may excel in their specific area, no one is addressing the car—or you—as a whole.
This compartmentalization means patients are bounced between specialists, each focusing on a single symptom or body part. For instance, a patient with chronic pain may see a neurologist for their nerves, an orthopedist for their bones, and a physical therapist for their muscles. While each specialist provides valuable insights, the lack of integration often leaves patients feeling like no one is looking at the bigger picture. It’s exhausting and can lead to gaps in care.
Functional Medicine: A Whole-Person Approach
Functional medicine seeks to address these shortcomings by adopting a holistic approach to healthcare. Instead of isolating individual symptoms, functional medicine practitioners view the body as an interconnected system. They consider factors like lifestyle, nutrition, stress, and genetics to identify root causes of illness and promote long-term wellness.
This model shifts the focus from disease management to health optimization. A functional medicine practitioner isn’t just interested in alleviating a patient’s immediate complaint; they aim to restore balance and improve overall quality of life. Patients often report feeling heard and understood in ways they haven’t experienced in traditional medical settings.
The Path Forward
As the frustration with compartmentalized medicine grows, so does the demand for a more integrated approach. Functional medicine is leading the charge by bridging the gap between fragmented care and whole-person health. By combining the expertise of specialists with a unifying perspective, this approach has the potential to transform not only individual lives but also the healthcare system at large.
Both patients and doctors deserve better. Functional medicine offers a blueprint for a future where healthcare is about more than fixing parts—it’s about nurturing the whole person.
